2. 广西医科大学附属肿瘤医院麻醉科,广西南宁 530021
2. Department of Anesthesiology, the Affiliated Cancer Hospital of Guangxi Medical University, Nanning, Guangxi, 530021, China
目前肝癌治疗手段多样化,但手术仍是肝癌首选的治疗方法[1]。由于肝脏结构复杂,术中大出血是手术治疗的重大危险因素之一[2],而相应的输血需求也会增加。有研究表明,输注异体血引起不良反应和预后的风险会大大增加[3, 4]。控制术中出血和输血是肝切除术中关注的重点[5-7]。低容量性自体储血(Hypovolemic Phlebotomy,HP)是一种新颖的干预手段,有研究表明HP与肝切除术中出血量和异体血输注的减少密切相关[8-10],但其安全性和有效性仍待研究。本研究通过观察在肝癌肝脏部分切除术中应用HP对出血和输血的影响及其安全可靠性,为临床提供依据。
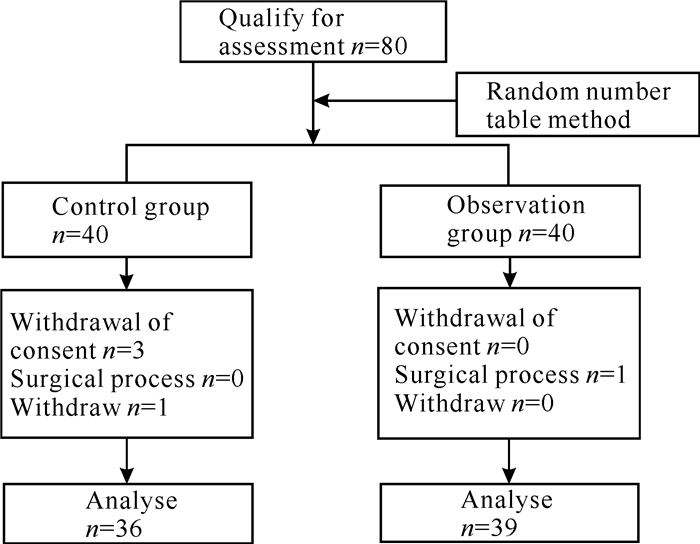
1 临床资料和方法 1.1 一般资料本研究获得广西医科大学附属肿瘤医院人类科学伦理委员会的同意批准(批准号:KY2018004),所有患者或家属已签署知情同意书,并在中国临床试验注册中心注册成功,注册号为ChiCTR180001734。选取2018年7月至2019年1月行开腹肝癌肝部分切除术的患者80例,年龄28-65岁,体质指数(Body Mass Index,BMI) 18-25 kg/m2,美国麻醉医师协会(American Society of Anesthesiologists,ASA)分级Ⅰ级或Ⅱ级,按照随机数字表法分成观察组(H组)和对照组(C组),H组40人,C组40人。纳入标准:术前诊断肝癌以及术后证实为肝癌;ASAⅠ、Ⅱ级;心功能Ⅰ、Ⅱ级;无严重慢性疾病;术前心、肝、肾、凝血功能无明显异常;术前血红蛋白110 g/L以上。排除标准:有凝血功能障碍或近期使用抗凝药物;二次肝癌手术者、术前已行放化疗治疗者;术中使用血管活性药物难以维持平均动脉压(Mean Arterial Pressure,MAP)≥60 mmHg者;临时改变手术方式;无法测量中心静脉压(Central Venous Pressure, CVP)者;数据记录不完整者。病例的具体纳入流程如图 1所示。
|
| 图 1 病例纳入流程图 Fig. 1 Flow chart of case inclusion |
1.2 方法
入室后给予患者心率(Heart Rate,HR)、血氧饱和度(Blood Oxygen Saturation,SPO2)、脑电双频指数(Bispectral Index,BIS)监护,开放颈内静脉及桡动脉。麻醉后,H组在开腹后切除肝实质前,根据体重计算采血量,采用微电脑采液控制器从桡动脉置管中精准缓慢采集占体重0.7%的全血,同时限制输液,不给予其他液体替代,以维持采血后的CVP在目标范围直至肝实质切除完毕。采集的血液储存在专用的血液采集袋。当肝癌组织切除完毕,即可开始液体复苏,同时回输血液,若出现血红蛋白≤70 g/L,先补液再回输自体血,若未改善再输注异体血。C组为对照组,不实行术中采血并常规输液,术中监测记录中心静脉压。
1.3 监测时点和指标记录麻醉前(T0)、麻醉后(T1)、开始采血时(T2)、采血完成时(T3)、开始切除肝脏前(T4)、肝癌切除并止血完成时(T5)、手术完成时(T6)的CVP、HR、MAP。记录术中出血量、采血量、手术前后血红蛋白(Hemoglobin,HBG)差值(△HBG)以及其他手术麻醉相关情况、一般资料。记录术前、术后第7天(T7)的肝功能[总胆红素(Total Bilirubin,TBIL)、直接胆红素(Direct Bilirubin,DBIL)、间接胆红素(Indirect Bilirubin,IBIL)、丙氨酸氨基转换酶(Alanine Aminotransferase,ALT)、门冬氨酸氨基转换酶(Aspartate Aminotransferase,AST)、白蛋白(Albumin,ALB)]、肾功能[尿素氮(Blood Urea Nitrogen,BUN)、肌酐(Creatinine,Cr)、肾小球滤过率(Glomerular Filtration Rate,GFR)],凝血功能[凝血酶原时间(Prothrombin Time,PT)、活化部分凝血活酶时间(Activated Partial Thromboplastin Time,APTT)、纤维蛋白原(Fibrinogen,FIB)、D-二聚体(D-dimer,DD)]、术后院内并发症、入住ICU时间、总住院时间以及术后住院时间。
1.4 统计学分析应用SPSS 17.0软件进行统计学分析。对计量资料进行正态性检验,符合正态分布的资料采用均数±标准差(x±s)表示,两组间比较采用两独立样本t检验;非正态分布的资料用中位数[四分位数,M(Q1,Q3)]表示,两组间比较采用两独立样本的Wilcoxon秩和检验,统计值为z值;计数资料采用χ2检验。P<0.05为差异有统计学意义。
2 结果与分析 2.1 两组患者的资料比较两组患者的一般资料(性别、年龄、身高、体重、体质指数)、手术麻醉相关资料(肝肿瘤位置、Child-pugh评分、ASA分级、丙泊酚、瑞芬、芬太尼、手术时间、输液量、尿量、△乳酸)比较差异无统计学意义(P > 0.05,表 1),结果提示临床观察过程中能够排除患者自身因素和手术麻醉因素对观察因素的影响。
| 项目 Items |
C组(n=36) C group (n=36) |
H组(n=39) H group (n=39) |
t/z/χ2值 t/z/χ2 value |
P值 P value |
| Gender (male/female) | 28/8 | 37/2 | 3.370 | 0.060 |
| Age (years) | 51.22±9.75 | 48.56±10.16 | 0.514 | 0.252 |
| Height (cm) | 164.47±7.49 | 166.85±6.08 | 2.091 | 0.135 |
| Weight (kg) | 58.28±10.13 | 62.26±10.13 | 0.200 | 0.093 |
| BMI (kg/m2) | 21.33±2.88 | 22.31±3.03 | 0.967 | 0.156 |
| Location of liver tumor (left/right/other) | 8/26/2 | 11/25/3 | 0.574 | 0.750 |
| Child-pugh scores | 5.00(5.00,6.00) | 5.00(5.00,5.00) | -0.898 | 0.369 |
| ASA classification (Ⅰ/Ⅱ) | 21/15 | 24/15 | 0.080 | 0.777 |
| Propofol (mg) | 1 218.06±373.12 | 1 286.26±422.08 | 0.155 | 0.462 |
| Remifentanil (μg) | 1 412.50±553.86 | 1 466.92±434.90 | 5.138 | 0.639 |
| Fentanyl (mg) | 500.00(450.00,500.00) | 500.00(450.00,500.00) | -0.711 | 0.477 |
| Operative time (min) | 220.89±68.16 | 208.08±56.07 | 0.638 | 0.375 |
| Fluid infusion volume (mL) | 2 487.50±880.93 | 2 135.90±672.67 | 2.070 | 0.053 |
| Urinary volume (mL) | 354.86±231.68 | 267.18±163.06 | 6.200 | 0.060 |
| △Lactate | -0.27±0.84 | -0.31±0.89 | 0.091 | 0.863 |
| Note: △Lactate=lactate before anesthesia-lactate at the end of surgery | ||||
2.2 两组患者术中CVP的比较
T2、T3时点H组的CVP平均降低2.27 cmH2O,即HP后CVP明显降低,提示HP能够有效降低CVP。T4、T5时点H组的CVP低于C组(P<0.01,表 2),说明在肝癌组织切除期间HP能够维持患者的CVP在一个较低的水平。
| 时点 Point in time |
C组(n=36) C group (n=36) |
H组(n=39) H group (n=39) |
t值 t value |
P值 P value |
| T0 | 6.63±2.64 | 7.20±2.36 | 0.216 | 0.327 |
| T1 | 7.02±3.12 | 6.61±2.24 | 2.427 | 0.520 |
| T2 | 7.67±2.59 | |||
| T3 | 5.40±2.43 | |||
| T4 | 7.68±2.83 | 4.80±2.21 | 1.671 | 0.000 |
| T5 | 7.99±2.53 | 5.42±2.22 | 0.744 | 0.000 |
| T6 | 9.11±2.46 | 9.75±2.88 | 0.654 | 0.306 |
2.3 两组患者出血和输血相关的比较
C组平均出血量为300 mL,H组平均出血量为200 mL,H组出血量低于C组(P<0.05),HP能够降低患者术中出血量,C组有3例异体输血,而H组无异体输血,可能与自体血储存有关(表 3)。
| 项目 Items |
C组(n=36) C group (n =36) |
H组(n =39) H group (n =39) |
t/z/χ2值 t/z/χ2 value |
P值 P value |
| Bleeding volume (mL) | 300(200,400) | 200(150,300) | -2.371 | 0.018 |
| △HBG (g/L) | 15.39±10.29 | 15.59±10.71 | 0.092 | 0.934 |
| △CVP (cmH2O) | 2.27±1.64 | |||
| HP collect-blood volume (mL) | 450 | |||
| Intraoperative transfusion of allogeneic blood (case) | 3 | 0 | 3.385 | 0.066 |
| Note: △CVP=CVP before blood collection-CVP after blood collection;△HBG=preoperative hemoglobin-postoperative day hemoglobin | ||||
2.4 两组患者术中HR、MAP的比较
与C组相比,H组患者术中各时间点HR、MAP无明显改变(P>0.05,表 4),由此可见HP对患者术中血流动力学无明显影响,说明HP后患者术中血流动力比较平稳。
| 项目 Items |
时点 Point in time |
C组(n=36) C group (n=36) |
H组(n=39) H group (n=39) |
t值 t value |
P值 P value |
| HR | T0 | 74.92±11.73 | 72.26±11.82 | 0.627 | 0.332 |
| T1 | 70.61±11.42 | 67.15±10.57 | 0.661 | 0.178 | |
| T4 | 78.25±12.68 | 72.38±10.94 | 0.051 | 0.219 | |
| T5 | 74.86±10.49 | 78.90±8.22 | 2.370 | 0.067 | |
| T6 | 70.33±8.32 | 71.77±10.05 | 0.496 | 0.505 | |
| MAP | T0 | 94.19±8.27 | 96.92±7.63 | 0.140 | 0.142 |
| T1 | 78.78±12.75 | 74.46±13.86 | 0.996 | 0.825 | |
| T4 | 87.42±10.92 | 98.08±14.60 | 0.595 | 0.227 | |
| T5 | 82.82±8.20 | 85.69±9.64 | 0.625 | 0.079 | |
| T6 | 85.89±9.46 | 89.36±8.42 | 0.843 | 0.097 |
2.5 两组患者术前术后重要脏器功能的比较
两组间术前、术后第7天时点的肝功能、肾功能、凝血功能、血小板比较无统计学差异(P>0.05,表 5),说明HP对患者术后重要脏器功能未产生明显的影响。
| 项目 Items |
时间 Time |
C组(n=36) C group (n=36) |
H组(n=39) H group (n=39) |
t值 t value |
P值 P value |
| TBIL | Preoperation | 17.26±7.82 | 16.10±6.37 | 1.001 | 0.478 |
| 7 d postoperatively | 27.22±13.54 | 22.90±9.79 | 3.024 | 0.115 | |
| IBIL | Preoperation | 11.05±5.79 | 9.48±3.48 | 3.113 | 0.156 |
| 7 d postoperatively | 14.28±8.17 | 11.55±6.21 | 2.005 | 0.107 | |
| DBIL | Preoperation | 7.94±5.39 | 6.03±2.60 | 7.671 | 0.060 |
| 7 d postoperatively | 13.69±6.83 | 11.73±8.85 | 0.109 | 0.289 | |
| ALB | Preoperation | 35.54±3.25 | 36.85±5.07 | 0.453 | 0.195 |
| 7 d postoperatively | 30.45±2.90 | 31.73±3.44 | 1.321 | 0.087 | |
| AST | Preoperation | 66.40±50.12 | 53.82±38.04 | 1.220 | 0.223 |
| 7 d postoperatively | 63.97±29.06 | 53.36±19.90 | 7.712 | 0.072 | |
| ALT | Preoperation | 74.76±79.62 | 56.67±44.37 | 3.672 | 0.226 |
| 7 d postoperatively | 106.31±86.92 | 104.13±60.41 | 1.723 | 0.899 | |
| CR | Preoperation | 74.86±16.08 | 81.44±14.04 | 2.726 | 0.063 |
| 7 d postoperatively | 69.75±18.75 | 73.15±19.45 | 0.258 | 0.444 | |
| BUN | Preoperation | 4.92±1.44 | 5.16±1.38 | 0.019 | 0.464 |
| 7 d postoperatively | 4.70±2.69 | 4.46±1.58 | 5.306 | 0.639 | |
| GFR | Preoperation | 87.72±28.89 | 82.36±19.80 | 2.014 | 0.559 |
| 7 d postoperatively | 97.67±20.40 | 103.22±25.82 | 0.454 | 0.343 | |
| PLT | Preoperation | 200.36±83.29 | 197.41±25.82 | 0.247 | 0.865 |
| 7 d postoperatively | 213.47±107.22 | 207.13±73.77 | 3.860 | 0.765 | |
| PT | Preoperation | 12.3±1.28 | 11.87±0.95 | 4.700 | 0.097 |
| 7 d postoperatively | 13.41±1.70 | 12.84±1.21 | 4.845 | 0.094 | |
| APTT | Preoperation | 27.52±4.54 | 25.87±3.06 | 5.868 | 0.067 |
| 7 d postoperatively | 30.46±7.13 | 29.21±10.07 | 0.094 | 0.541 | |
| FIB | Preoperation | 2.97±1.02 | 2.72±0.76 | 4.340 | 0.219 |
| DD | 7 d postoperatively | 2.44±1.56 | 3.08±1.32 | 0.001 | 0.059 |
| D-dimer | Preoperation | 0.93±0.78 | 0.68±0.44 | 11.150 | 0.090 |
| 7 d postoperatively | 7.38±2.79 | 7.55±4.09 | 5.554 | 0.819 |
2.6 两组患者的围术期情况比较
两组患者总住院时间、术后住院时间、二期缝合及术后胸腔积液情况的比较均无统计学差异(P>0.05,表 6),提示HP对患者术后短期恢复无不良影响。
| 项目 Items |
C组(n=36) C group (n=36) |
H组(n=39) H group (n=39) |
t/χ2值 t/χ2 value |
P值 P value |
| Total hospital stay (d) | 19.94±5.51 | 18.56±4.60 | 0.170 | 0.242 |
| Postoperative hospital stay (d) | 9.67±2.87 | 10.60±3.47 | 0.405 | 0.169 |
| Secondary suture (case) | 1 | 1 | 0.003 | 0.954 |
| Postoperative pleural effusion (case) | 0 | 1 | 0.936 | 0.333 |
3 讨论
Hashimoto等[11]于2007年在肝脏分离前放出了占体重0.7%的全血,使得出血量明显减少,首次引进了标准化HP的概念。与Hashimoto等[11]的观察结果一致,本研究观察到HP组出血量比对照组明显减少。Rekman等[12]选择了术前采血4.7-10 mL/kg,结合其他措施维持CVP < 5 cmH2O,发现术中失血量显著减少。本研究采用标准化HP,采集占体重0.7%的全血,HP后主要通过限制输液维持采血后的CVP在目标范围内直至肝癌切除并止血完成,并未全部要求CVP < 5 cmH2O。结果表明实行HP能有效减少术中出血。Ryckx等[13]回顾分析了100例肝移植病例,发现HP后可使CVP下降,术中出血量可降低至165 mL。本研究发现HP后CVP平均降低2.27 cmH2O,且T4、T5时点H组的CVP比C组显著降低,即整个肝实质切除过程,H组的CVP维持在一个较低的状态,这也是实行HP能有效减少术中出血的原因。
术中出血过多的必然结果是术中或术后输血量的增加。而肝癌肝切除术相关的病例回顾分析发现,影响患者预后的独立危险因素包含术中或术后输血[14-16]。Al Khaldi等[9]和Park等[8]研究发现HP与肝脏手术患者输血减少有关,本研究也发现H组无异体输血的病例,可能与切肝前行HP减少术中出血相关,同时储备自体血有利于降低输注异体血的风险。而自体血的储备和回输是血液保护的关键所在[17],故HP有利于血液保护。
区别于急性等容量血液稀释[18]、急性高容量血液稀释[19]两种血液保护方法,HP的特点是放出自身血液后不使用其他液体替代,直至切除肝实质完毕后再回输自体血液。肝脏手术出血主要在于切除肝实质的过程,本研究选择麻醉开腹后在切除肝实质前进行采血,目的是减少血流动力学波动的时间。当急性失血不足全身血容量的15%时[20],机体可通过自身代偿。按照体重的0.7%实行HP,并未超出血容量的15%。虽然C组有1例、H组有2例患者使用了去甲肾上腺素,但是术中生命体征较为平稳,H组39例患者均在安全可控的条件下顺利完成手术,说明HP在短时间内不会导致血流动力学的剧烈波动。
有关HP的争议是低血容量是否容易导致脏器灌注不足,增加术后并发症。Ryckx等[13]只提到HP后对肾功能无明显影响。本研究追踪了肝功能、肾功能、凝血功能、血小板多个脏器和系统情况,所有患者在住院期间未发生上述重要脏器功能衰竭。与术前相比,HP未增加对终末器官脏器的损伤。两组术后情况无明显差异,说明HP术后未引起严重并发症,对患者术后康复未产生不良影响。
本研究也存在局限。首先是样本例数过少,虽然样本量少,但是研究前期查阅有关肝癌肝切除术的临床观察研究[21-23]所选取的样本量小也能得到有意义的结论;其次是没有严格控制CVP低于5 cmH2O,但是我们发现H组的CVP均维持在一个较低的水平,能够有效减少术中失血,因此并不一定要严格控制CVP低于5 cmH2O,应结合实际情况进行操作。
4 结论综上所述,HP在肝癌肝部分切除术中可以降低中心静脉压进而减少术中出血量,自体血回输减少了输注异体血相关的风险;HP后,术中及术后无严重并发症发生,对重要脏器功能无明显损伤。该技术的应用是安全可靠的,故推荐在肝癌肝部分切除术中使用HP以减少术中出血量和异体血的输注。
| [1] |
朱鹏, 陈孝平. 我国肝癌肝切除技术发展之路[J]. 中国实用外科杂志, 2021, 41(7): 721-724. DOI:10.19538/j.cjps.issn1005-2208.2021.07.01 |
| [2] |
PAN Y X, WANG J C, LU X Y, et al. Intention to control low central venous pressure reduced blood loss during laparoscopic hepatectomy: A double-blind randomized clinical trial[J]. Surgery, 2020, 167(6): 933-941. DOI:10.1016/j.surg.2020.02.004 |
| [3] |
YAO L Q, CHEN Z L, FENG Z H, et al. Clinical features of recurrence after hepatic resection for early-stage hepatocellular carcinoma and long-term survival outcomes of patients with recurrence: A multi-institutional analysis[J/OL]. (2022-02-22)[2022-03-22]. http://doi.org/10.1245/s10434-022-11454-y.
|
| [4] |
KARANICOLAS P J, LIN Y, MCCLUSKEY S, et al. Tranexamic acid versus placebo to reduce perioperative blood transfusion in patients undergoing liver resection: protocol for the haemorrhage during liver resection tranexamic acid (HeLiX) randomised controlled trial[J]. BMJ Open, 2022, 12(2): e058850. DOI:10.1136/bmjopen-2021-058850 |
| [5] |
GRATZ J, ZOTTI O, PAUSCH A, et al. Effect of goal-directed crystalloid versus colloid administration on perioperative hemostasis in partial hepatectomy: A randomized, controlled trial[J]. Journal of Clinical Medicine, 2021, 10(8): 1651. DOI:10.3390/jcm10081651 |
| [6] |
XIAO L K, HUANG P, WU K, et al. Effect of infrahepatic inferior vena cava partial clamping on central venous pressure and intraoperative blood loss during laparoscopic hepatectomy[J]. Surgical Endoscopy, 2021, 35(6): 2773-2780. DOI:10.1007/S00464-020-07709-y |
| [7] |
舒强, 刘小玲, 徐波. Glisson蒂横断法与Pringle法在肝细胞癌肝切除术中的应用效果Meta分析[J]. 中国普通外科杂志, 2022, 31(1): 42-54. |
| [8] |
PARK L, GILBERT R, BAKER L, et al. The safety and efficacy of hypovolemic phlebotomy on blood loss and transfusion in liver surgery: A systematic review and meta-analysis[J]. HPB, 2020, 22(3): 340-350. DOI:10.1016/j.hpb.2019.10.001 |
| [9] |
AL KHALDI M, GRYSPEERDT M F, CARRIER F M, et al. Effect of intraoperative hypovolemic phlebotomy on transfusion and clinical outcomes in patients undergoing hepatectomy: A retrospective cohort study[J]. Canadian Journal of Anaesthesia, 2021, 68(7): 980-990. DOI:10.1007/s12630-021-01958-8 |
| [10] |
MARTEL G, BAKER L, WHERRETT C, et al. Phlebotomy resulting in controlled hypovolaemia to prevent blood loss in major hepatic resections (PRICE-1): A pilot randomized clinical trial for feasibility[J]. The British Journal of Surgery, 2020, 107(7): 812-823. DOI:10.1002/bjs.11463 |
| [11] |
HASHIMOTO T, KOKUDO N, ORII R, et al. Intraoperative blood salvage during liver resection: A randomized controlled trial[J]. Annals of Surgery, 2007, 245(5): 686-691. DOI:10.1097/01.sla.0000255562.60215.3b |
| [12] |
REKMAN J, WHERRETT C, BENNRTT S, et al. Safety and feasibility of phlebotomy with controlled hypovolemia to minimize blood loss in liver resections[J]. Surgery, 2017, 161(3): 650-657. DOI:10.1016/j.surg.2016.08.026 |
| [13] |
RYCKX A, CHRISTIAENS C, CLARYSSE M, et al. Central venous pressure drop after hypovolemic phlebotomy is a strong independent predictor of intraoperative blood loss during liver resection[J]. Annals of Surgical Oncology, 2017, 24(5): 1367-1375. DOI:10.1245/s10434-016-5737-7 |
| [14] |
PAPADOPOULOU K, DOROVINIS P, KYKALOS S, et al. Short-term outcomes after robotic versus open liver resection: A systematic review and meta-analysis[J]. Journal of Gastrointestinal Cancer, 2022, 53(1): 1-10. DOI:10.1007/s12029-022-00810-6 |
| [15] |
夏永祥, 张峰, 李相成, 等. 原发性肝癌10966例外科治疗分析[J]. 中华外科杂志, 2021, 59(1): 6-17. |
| [16] |
YANG T, LIU K, LIU C F, et al. Impact of postoperative infective complications on long-term survival after liver resection for hepatocellular carcinoma[J]. The British Journal of Surgery, 2019, 106(9): 1228-1236. DOI:10.1002/bjs.11231 |
| [17] |
WELLER A, SEYFRIED T, AHRENS N, et al. Cell salvage during liver transplantation for hepatocellular carcinoma: A retrospective analysis of tumor recurrence following irradiation of the salvaged blood[J]. Transplantation Proceedings, 2021, 53(5): 1639-1644. DOI:10.1016/j.transproceed.2021.03.025 |
| [18] |
NI Y, DING X H, XU Z J, et al. Association of acute normovolemic hemodilution with decreased length of hospital stay in rhesus-negative patients undergoing major cancer surgeries: A retrospective study[J]. Annals of Palliative Medicine, 2021, 10(2): 1815-1824. DOI:10.21037/apm-20-1327 |
| [19] |
WU J, ZHANG Z. The effects of acute hypervolemic hemodilution and conventional infusion in laparoscopic radical prostatectomy patients[J]. American Journal of Translational Research, 2021, 13(7): 7866-7873. |
| [20] |
DIVERS T J, RADCLIFFE R M, COOK V L, et al. Calculating and selecting fluid therapy and blood product replacements for horses with acute hemorrhage[J]. Journal of Veterinary Emergency and Critical Care, 2022, 32(S1): 97-107. DOI:10.1111/vec.13127 |
| [21] |
张浩, 董科, 俞小炯, 等. 完全腹腔镜和开腹肝切除手术治疗原发性肝细胞肝癌的近期和远期疗效比较[J]. 实用医学杂志, 2017, 33(12): 1943-1948. DOI:10.3969/j.issn.1006-5725.2017.12.012 |
| [22] |
邓维, 李强, 张睿杰, 等. 开腹肝癌切除术与腹腔镜肝癌切除术治疗肝细胞癌患者临床疗效的比较[J]. 中国老年学杂志, 2016, 36(17): 4226-4228. DOI:10.3969/j.issn.1005-9202.2016.17.044 |
| [23] |
顾云霞, 邓福谋, 邓美玲, 等. 丹参酮ⅡA磺酸钠后处理联合控制性低中心静脉压对肝脏缺血-再灌注损伤的影响[J]. 临床麻醉学杂志, 2017, 33(7): 632-636. DOI:10.3969/j.issn.1004-5805.2017.07.002 |



